This disease is on the rise—and many people don’t know that they have it
Nine out of 10 people with chronic kidney disease only find out when it progresses to later stages. Here’s what we know about its risk factors—and why there's new reason to hope for more effective treatments.
When Alex Simmons was 37, he found himself in the emergency room with cramps, migraines, and a tight feeling in his stomach. Simmons, who lives in Pittsburgh and works as a personal trainer, had been feeling tired and run-down for about a month leading up to his hospitalization, which he brushed off, thinking he was just coming down with a virus.
Then, Simmons started getting sicker, to the point that he could no longer ignore his symptoms. When the doctors measured his blood pressure, it was 260/150, a number that shocked all of them, given that Simmons was young and in excellent shape.
As it turned out, Simmons had advanced chronic kidney disease, which rapidly progressed to kidney failure. “I was in the hospital for two weeks, and left on dialysis,” Simmons says.
An estimated 700 million people worldwide have chronic kidney disease—including 35.5 million people in the United States, or 15 percent of the population. However 9 out of 10 people don’t know that they have it, often only finding out when they are in the later stages of the disease. “There is no kidney pain that comes with kidney disease, so you don’t know you have it,” says Samir Parikh, a nephrologist at UT Southwestern Medical Center.
(How pig transplants are giving hope to kidney disease patients.)
Chronic kidney disease is also on the rise, in a trend that has many researchers and physicians stumped as to the full reasons for why this is—and also has them worried given the link between kidney disease and heart disease, the leading cause of death globally.
The good news is that there has been an influx of new treatments for most forms of chronic kidney disease, which means that if it is caught early, there are a number of options that can help. “It’s a tremendous time of innovation, not just for common forms of CKD, but also for kidney disease of less uncommon origins,” Parikh says.
What causes chronic kidney disease?
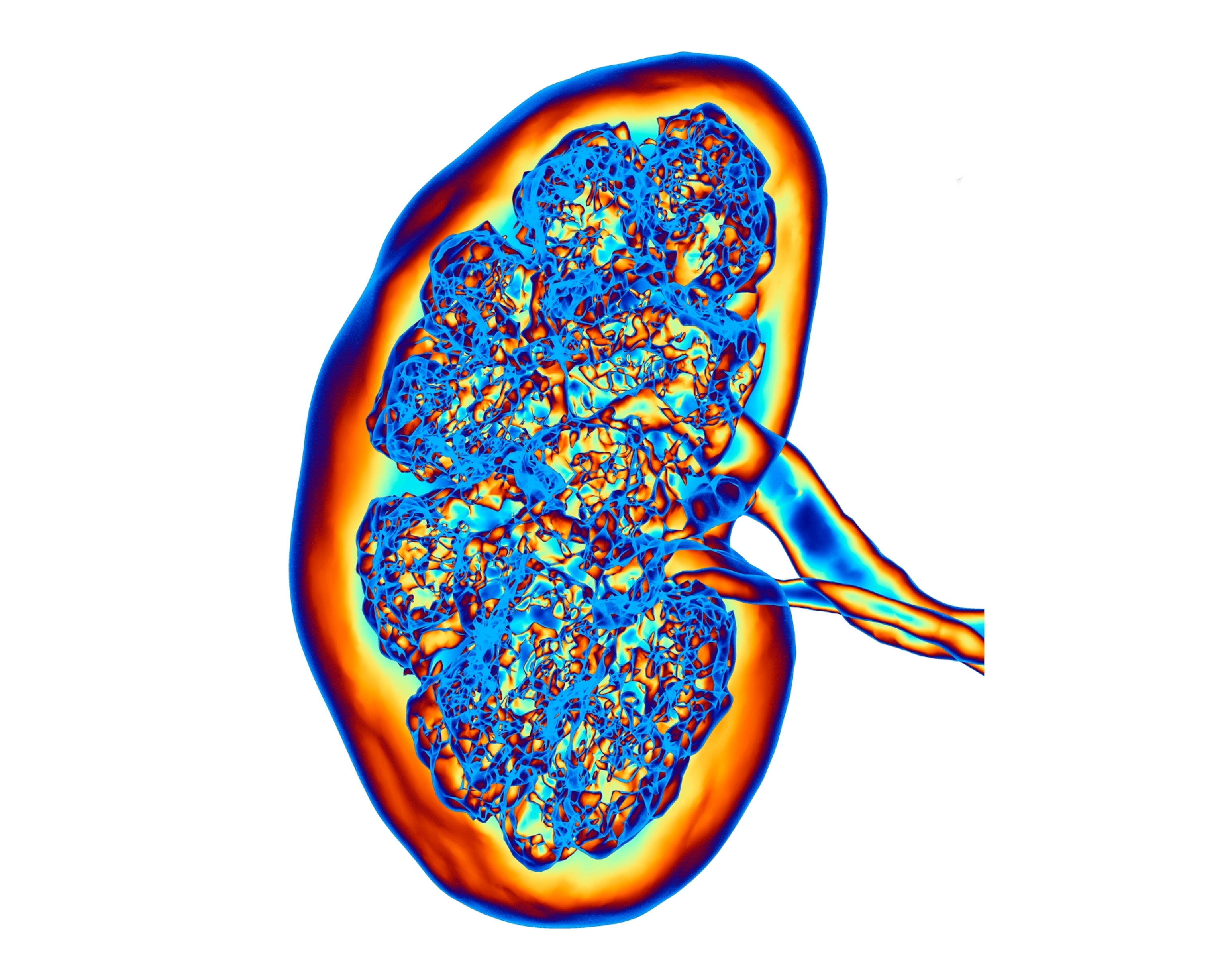
The kidneys are responsible for filtering our blood, removing toxins and keeping its beneficial compounds. They also play an important role in regulating the amount of fluid in our bodies, ensuring that enough blood cells are made, and controlling blood pressure.
“The kidneys are a bunch of small blood vessels that form these microscopic filters,” Parikh says. The problem, Parikh says, is that these filters can’t be replaced, which means that “the filters you are born with have to last a lifetime.” If these blood vessels get damaged, then the kidneys lose their ability to function properly.
Some of the common conditions that can cause kidney damage include diabetes, high blood pressure, obesity, and autoimmune diseases such as lupus or IgA nephropathy, also known as Berger disease. There are also some common medications, such as NSAIDs and antacids, that can damage the kidneys if taken for too long. People are also at greater risk if they have a family history of kidney disease.
(It’s possible to reverse diabetes—and even faster than you think.)
Chronic kidney disease on the rise
There are more than 600 million people worldwide living with kidney disease, which represents a 90 percent increase since 1990. The prevalence of kidney disease varies worldwide, with higher rates found in countries where healthcare access is an issue.
This increase is thought to be due to several factors, the first being a rise in chronic conditions, such as hypertension and type 2 diabetes, that put people at risk for developing chronic kidney disease.
Meanwhile other risk factors include exposure to environmental toxins, such as air pollution and water contamination—which is especially a concern in developing countries. The third factor is the overuse of medications, such as antacids and non-steroidal anti-inflammatory drugs, that can damage the kidneys.
“A large part can be explained by the increase in risk factors, but not all of them,” says Joachim Jankowski, a researcher at Maastricht University, in Maastricht, Netherlands. “Some is unknown.” Other factors that are thought to be linked to the rise in kidney disease include climate change, as extreme heat events can damage the kidneys, and healthcare disparities, as a lack of healthcare can cause or worsen kidney disease.
The threat of undiagnosed chronic kidney disease
The biggest health risk associated with chronic kidney disease is dying of heart disease. “Patients who have CKD have an increased risk for all forms of cardiovascular disease,” says Brad Rovin, a nephrologist at The Ohio State University Wexner Medical Campus. “The epidemiology of the link is very, very clear.”
Although death from heart disease has been decreasing in recent decades, as result of improved medical care and reduction in risk factors, heart disease is still the leading cause of death globally. Experts suspect the reason for this may well be due to undiagnosed chronic kidney disease, which puts people at a much higher risk for dying of heart disease.
“The overall cardiovascular mortality of the population is not decreasing, it’s quite stable,” Jankowski says. “At the moment, we believe that the cardiovascular diseases are caused by kidney diseases, and the cardiovascular diseases are a consequence of the kidney diseases.”
(Why heart attacks are rising in young adults—and what to watch out for.)
Chronic kidney disease also comes with a number of other health concerns that may not seem connected to the kidneys, but actually are—such as high blood pressure, high cholesterol or nerve damage. “It’s a lot of symptoms that come with the disease,” says Stephanie Corona, who has polycystic kidney disease and is currently in end-stage renal failure. “You feel sick constantly.”
These health issues can occur because the kidney is responsible for maintaining a lot of our bodily functions, such as controlling our blood pressure and fluid levels. When that process starts to fail, a lot of other issues develop as a result. “The kidney is the center of homeostasis balance,” says Katherine Tuttle, a nephrologist at the University of Washington Providence Medical Research Center. “When your kidneys go, everything goes awry.”
How to detect kidney disease
For people who have any of the risk factors for kidney disease, it’s important to get checked regularly, and to stay on top of any health conditions that can lead to kidney damage.
The two main tests for kidney function are a urine test, which looks for the presence of a protein called albumin to reveal how leaky these blood vessels are, and a blood test, which tests for a substance called creatinine, which can be used to estimate how well the kidneys are filtering the blood.
“Don’t be afraid to know your numbers,” Parikh says. “We’re really good at finding kidney disease if we get the chance to find it.”
Experts say early detection is key to slowing the progression of kidney damage—especially now with the rise of promising new treatments.
An era of innovation for kidney disease
Until recently, there were only limited treatment options for kidney disease, mainly dialysis or a kidney transplant. However, there has been an explosion of new therapies in recent decades. This includes treatments for the genetic disease polycystic kidney disease and treatments that can selectively target autoimmune diseases that damage the kidneys.
For patients whose kidney disease developed as a result of high blood pressure or type 2 diabetes, there are two new classes of diabetes drugs that have been shown to preserve kidney function while also reducing the risk of cardiovascular disease. “There is this emerging theme that what is good for the kidney is good for the heart, and what is good for the heart is good for the kidney,” Parikh says.
These new drugs include GLP-1 receptor agonists like Ozempic and Wegovy. A recent clinical trial investigating the benefits of Ozempic for diabetic chronic kidney disease was even stopped early because the death rate in the group receiving Ozempic was so much lower than the placebo group that it was no longer considered ethical to continue giving participants the placebo.
(The unexpected health benefits of Ozempic and Mounjaro.)
SGLT2 inhibitors, the other new class of drug, also show a similar effectiveness at preserving kidney function, and reducing the risk of cardiovascular disease. There’s emerging evidence, too, that combining these treatments with GLP-1s can have an additive effect.
“You can really dramatically slow down the rate of progression,” Parikh says. “We’re talking a difference of decades.” This includes saving patients from reaching end-stage renal disease, when they would need either dialysis or a kidney transplant, as well as protecting against dying of a heart attack or stroke.
Simmons knows firsthand the benefits of getting tested. He survived kidney failure after receiving a new one from his sister, inspiring him to help raise awareness about the disease. His top advice? Staying up-to-date on your medical care, including annual wellness checks, even if you believe you’re completely healthy. “Get your labs done,” Simmons says.